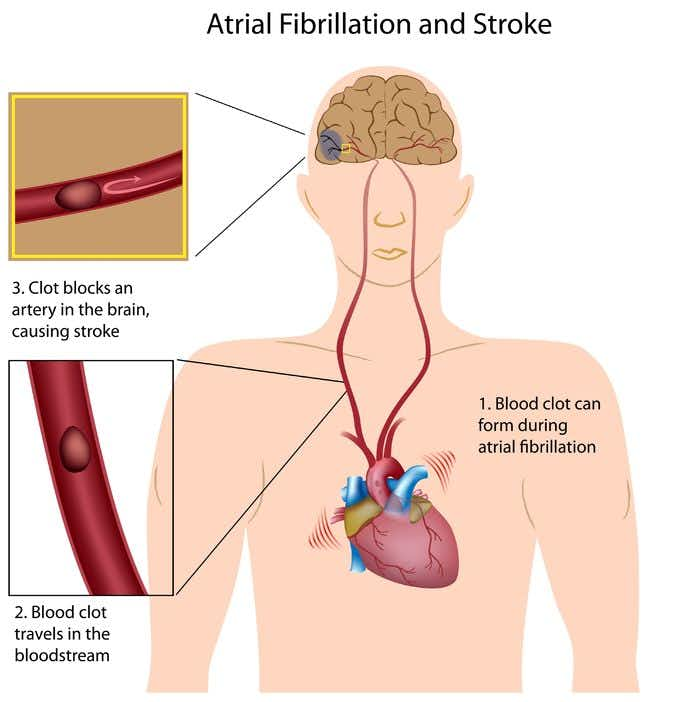
This case takes place in Nevada and involves a 65-year-old woman who suffered a stroke secondary to clot in the setting atrial fibrillation. Her past medical history included hypertension, hyperlipidemia, atrio-septal defect repair and obstructive sleep apnea which had been treated with a Pillar Procedure. 2-years ago she was diagnosed with atrial fibrillation with pulpmary vein isolation and ablation, and had subsequently been started on Coumadin by her cardiologist. The cardiologist performed a cardioversion and subsequently discontinued her anti-coagulation medication. She had a follow-up with cardiology 6-months after her diagnosis and it was noted that she had no recurrence of atrial fibrillation. 18-months later, the patient suffered a stroke secondary to clot developed in the setting of atrial fibrillation. She was administered TPA but experienced no meaningful resolution of her left sided paralysis. Of note, she developed mild hemorrhagic conversion secondary to the TPA. Her treatment records subsequent to the stroke indicate the patient has chronic atrial fibrillation. They also note the patient was not on anti-coagulation prior to the stroke and that it had been discontinued by her cardiologist. Presently, the patient has total left sided paralysis, speech impairment, and is wheelchair bound.
Question(s) For Expert Witness
1. How often do you treat patients with atrial fibrillation?
2. What is the recommended anti-coagulation regimen for these patients?
3. What are the indications for discontinuation of anti-coagulation in these patients?
Expert Witness Response E-007032
I treat patients with atrial fibrillation daily. Anticoagulation is indicated based on certain baseline risk factors and comorbidities that each patients has. If the patient has none of these specific risk factors, it is reasonable not to treat atrial fibrillation with anticoagulation. This is based on certain scores (CHADS or CHADS VAS score). If these scores are low (<2), a reasonable alternative would be aspirin therapy. There are instances where anticoagulation can be stopped. One example would be in the case of a patient with no significant risk factors for stroke who has been on Coumadin for four weeks after cardioversion. It does not appear that these scores were monitored in this specific case. An in-depth review of the records is required to assess the CHADS and CHADS VAS scores.
About the author
Michael Morgenstern
Michael is Senior Vice President of Marketing at The Expert Institute. Michael oversees every aspect of The Expert Institute’s marketing strategy including SEO, PPC, marketing automation, email marketing, content development, analytics, and branding.