This case involves a ten-year-old male patient, who originally presented to his primary care physician with generalized malaise and symptoms that would generally point towards an infectious etiology. The primary care physician took a limited history on the initial visit and did not examine the patient, reassuring the patient’s parents that his condition was most likely self-limiting and would resolve soon. The physician remained dismissive when the patient returned shortly after the initial visit complaining of the same symptoms. It was not until the patient’s third trip to the medical practice that the physician examined him. On examination, the treating physician found an enlarged axillary lymph node that he felt required further investigation. The patient was referred to a local children’s hospital. The treating physician ordered a work-up which included the sampling of the lymphatic gland. The lymph node biopsy confirmed infection. Soon after the minor surgical procedure the patient crashed and was taken to the ICU. He was diagnosed with Lemierre’s disease. The patient was resuscitated and remained in hospital for a long period of time before being discharged. Upon arriving at home after discharge, the patient broke out in a rash and was taken to the ER once again. The patient was eventually diagnosed with Stevens–Johnson syndrome and died during his last admission from complications due to the disease process.
Question(s) For Expert Witness
1. Were there departures from the standard of care that led to patient developing Stevens-Johnson syndrome and his subsequent death?
Expert Witness Response E-000094
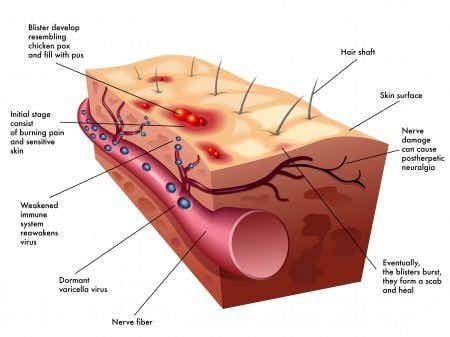
It appears from the description that the child had Lemierre's syndrome and had negative sequelae after lymph node biopsy and then received antibiotics - possibly trimethoprim-sulfamethoxazole - that led to Stevens-Johnson Syndrome. As such, unfortunately nothing could have been done to prevent Stevens-Johnson syndrome (unless the patient had a known history of adverse drug events with sulfa drugs - or whatever drug was thought to be the inciting drug). There is no clear treatment for Stevens-Johnson syndrome besides supportive care (fluids, wound care, etc.). Some physicians have tried steroids, intravenous immunoglobulins, plasmapheresis, etc but all of these therapies lack strong supportive evidence of their efficacy and some experts believe that they are harmful. Stevens-Johnson syndrome generally begins suddenly, my assumption is that it is unlikely that this child had symptoms prior to hospital discharge. Stevens-Johnson syndrome is usually related to antibiotics used. It is a serious disease with its own mortality, however, there is a possibility that the treatment given could have precipitated the patient’s death.
About the author
Dr. Faiza Jibril
Dr. Faiza Jibril has extensive clinical experience ranging from primary care in the United Kingdom, to pediatrics and child abuse prevention at Mount Sinai Hospital, to obstetrics in Cape Town, South Africa. Her post-graduate education centered on clinical research and medical ethics. Dr. Jibril is currently Head of Sales in the US and Canada for Chambers and Partners - a world leading legal ranking and insights intelligence company.