This case involves a seventy-four-year-old male, with a history significant for BPH, that presented to the emergency room after a syncopal episode. The patient also complained of upper back pain that was thought to be associated with rigorous physical activity the past few days. The patient reported becoming dizzy and sweating while lying in bed. He thought he was having a heart attack, but when he got up to take an aspirin, he passed out for a few minutes. The patient denied chest pain or shortness of breath on arrival, but did feel nauseous and vomited two times before coming to the hospital. While in the ER, the patient started to complain of right shoulder blade pain traveling to the front of his chest towards the neck. The patient was not worked up with the standard diagnostic tests for an aortic dissection or abnormal heart rhythms. Only a chest X-ray, EKG, and cardiac enzymes were ordered as part of a brief cardiac workup. The EKG showed a prolonged QT wave and also inverted T waves. The patient was admitted to the internal medicine floor for observation and within four hours of his admission, the patient sustained another syncopal episode while trying to ambulate. The patient was found by nursing staff and a code blue was called. CPR protocol was initiated but the patient was unable to be revived.
Question(s) For Expert Witness
1. What is the accepted method of diagnosis for an impending aortic dissection?
Expert Witness Response
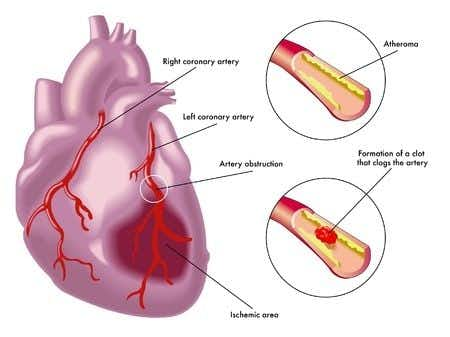
Patients with abdominal aortic dissection are at times asymptomatic, but in the cases where they are symptomatic, patients complain of abdominal, flank or back pain. If the patient is hemodynamically unstable, is it possible that the dissection ruptured. Aortic dissection is usually diagnosed by using cardiovascular imaging techniques before the result of blood work is interpreted. The choice of abdominal imaging techniques depends in part on whether or not the patient is hemodynamically stable. A chest x-ray is the initial imaging technique, which is neither sensitive nor specific for diagnosis. Abdominal ultrasound is the gold standard for diagnosis of non-ruptured AAA. If AAA is less than 5 cm, the patient can be medically managed (i.e. controlling comorbid conditions like hypertension). In the case where the patient has a ruptured AAA, then a CT scan should be done to evaluate the extent of rupture. If hemodynamically unstable and the patient is showing signs of instability, then emergent surgery is required.
About the author
Michael Talve, CEO
Michael Talve stands at the forefront of legal innovation as the CEO and Managing Director of Expert Institute. Under his leadership, the Expert Institute has established itself as a vital player in the legal technology arena, revolutionizing how lawyers connect with world-class experts and access advanced legal technology. Michael's role involves not only steering the company's strategic direction but also ensuring the delivery of unparalleled intelligence and cutting-edge solutions to legal professionals. His work at Expert Institute has been instrumental in enhancing the capabilities of attorneys in case preparation and execution, making a significant impact on the legal industry's approach to expert consultation and technological integration. Michael's vision and execution have positioned the Expert Institute as a key facilitator in the intersection of law and technology.