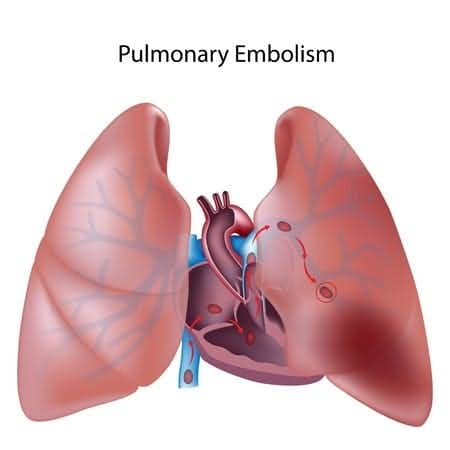
This case takes place in Minnesota and involves a 50-year-old male patient who presented to the ER with shortness of breath and chest tightness. The cardiologist who saw him felt the patient had undergone an acute coronary event. He underwent cardiac catheterization, which showed no significant coronary artery disease. An echocardiogram was done, which showed elevated right ventricular pressure. The pulmonologist saw the patient and noted “shortness of breath, increased BNP, most likely has obstructive sleep apnea.” A pillar procedure to mediate the apea was considered, but discarded by the doctors. A venous Doppler of the legs was ordered which came back as positive for deep vein thrombosis (DVT) from the common femoral vein down to the calf. The next day the patient complained of left-sided chest pain, noted to be tachypneic. Doctors considered a pulmonary vein isolation and ablation, but decided that the symptoms were too inconclusive. That evening he became acutely short of breath and was noted to be pale, dusky, and cyanotic. He coded and CPR was attempted, however he expired that evening. Of note, tPA was never given during his cardiac arrest. The plaintiff alleges the patient was misdiagnosed with acute coronary syndrome, CHF, and potential Antiphospholipid Syndrome even though he presented to the ER with signs and symptoms of pulmonary embolism.
Question(s) For Expert Witness
1. How often do you treat patients with these presenting complaints?
2. Based on the brief case summary, was the patient's signs and symptoms consistent with pulmonary embolism?
3. What are some tests to rule it out?
4. Were there any procedures that could have been taken to prevent his death?
Expert Witness Response
The patient's presenting signs and symptoms were consistent with pulmonary embolism, and that diagnosis should have been more strongly considered when the pulmonary hypertension was found. The patient should have been started on heparin immediately after the leg vein thrombosis was discovered. Thrombolysis should have been given when he was hypotensive. Prompt consideration of the diagnosis and treatment with anticoagulation and thrombolysis could have been life saving. Additional testing for pulmonary embolism would have included pulmonary VQ scan or chest CT angiography.
About the author
Michael Morgenstern
Michael is Senior Vice President of Marketing at The Expert Institute. Michael oversees every aspect of The Expert Institute’s marketing strategy including SEO, PPC, marketing automation, email marketing, content development, analytics, and branding.