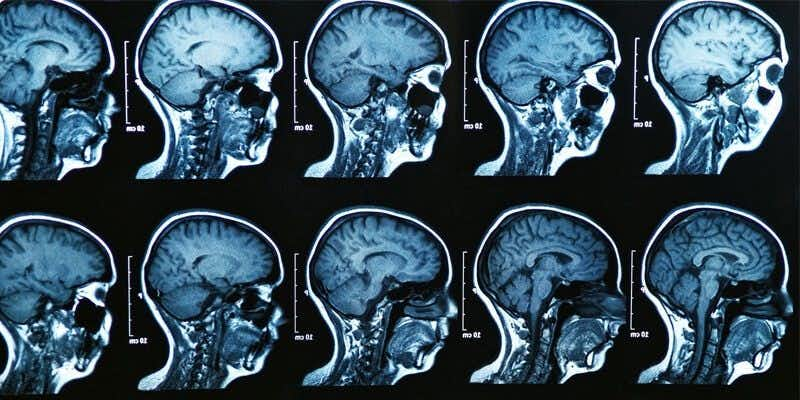
This case involves an 80-year-old male with a history of hypertension and paroxysmal atrial fibrillation. He had been off of the blood thinner Warfarin for several months when he presented to the emergency room with altered mental status. On initial exam, he was difficult to arouse with slurred speech and an expressive aphasia. A head CT was performed which did not reveal any acute intracranial abnormality. The primary differential diagnosis was an acute cerebrovascular accident due to the patient’s history of atrial fibrillation combined with his onset of neurologic deficits. A stat brain MRI was ordered but was not completed until the following day. In the meantime, the patient was admitted to the internal medicine service. Imaging revealed an acute infarct in the posterior temporal and occipital regions, bilateral cerebral peduncle infarcts, and a blot clot at the basilar terminus obstructing flow to the superior cerebellar arteries. The patient’s neurologic status continued to rapidly decline and he eventually succumbed to his injuries.
Question(s) For Expert Witness
1. How frequently do you treat patients suffering from acute CVAs?
2. When an MRI is ordered to be done STAT, what follow-up should occur to confirm that it was performed in a timely matter?
Expert Witness Response E-110048
I care for multiple stroke patients each year. Previously, I have been part of the acute stroke team at a major university-affiliated hospital responding to stroke alerts in the emergency department. I am a stroke researcher with an emphasis on strokes which occur to patients in the hospital and quality improvement for hospital systems that care for elderly patients. I have a number of publications and give presentations nationally on stroke quality of care, quality improvement, outcomes. I have reviewed cases of patients who experienced delays in obtaining timely imaging although primarily for quality improvement purposes.
A "stat" imaging study should be done with the highest priority. There can be external factors that impact the observed time from order to interpretation of the test. Acute stroke has a time-critical window in which the average stroke patient is losing millions of neurons per minute and hyperacute treatment is critical. After that critical window, the timing of the evaluation becomes less urgent as the emphasis changes from immediate breakup or removal of the clot to secondary prevention. Regarding the appropriate timeline to escalate if the imaging test was not returning in a timely fashion, this would depend on a number of factors -- most significantly, whether the results are needed for diagnosis that will change management versus confirmation of a suspected diagnosis that would not change immediate management but would impact long-term therapy decisions. I would also take into consideration whether there were alternative imaging modalities available that would provide the needed information. To answer the question of the medical appropriateness of the actual management in this case, I would need to review the documentation.
About the author
Wendy Ketner, M.D.
Dr. Wendy Ketner is a distinguished medical professional with a comprehensive background in surgery and medical research. Currently serving as the Senior Vice President of Medical Affairs at the Expert Institute, she plays a pivotal role in overseeing the organization's most important client relationships. Dr. Ketner's extensive surgical training was completed at Mount Sinai Beth Israel, where she gained hands-on experience in various general surgery procedures, including hernia repairs, cholecystectomies, appendectomies, mastectomies for breast cancer, breast reconstruction, surgical oncology, vascular surgery, and colorectal surgery. She also provided care in the surgical intensive care unit.
Her research interests have focused on post-mastectomy reconstruction and the surgical treatment of gastric cancer, including co-authoring a textbook chapter on the subject. Additionally, she has contributed to research on the percutaneous delivery of stem cells following myocardial infarction.
Dr. Ketner's educational background includes a Bachelor's degree from Yale University in Latin American Studies and a Doctor of Medicine (M.D.) from SUNY Downstate College of Medicine. Moreover, she is a member of the Board of Advisors for Opollo Technologies, a fintech healthcare AI company, contributing her medical expertise to enhance healthcare technology solutions. Her role at Expert Institute involves leveraging her medical knowledge to provide insights into legal cases, underscoring her unique blend of medical and legal acumen.