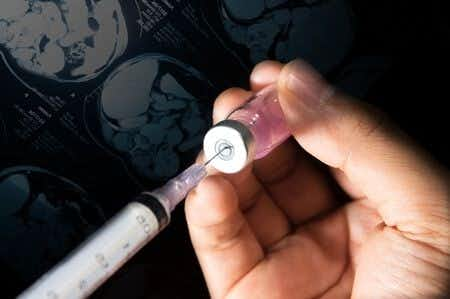
This case involves a 56-year-old female with a history of hypertension who presented with complaints of extremity and tongue numbness as well as slurred speech. Upon evaluation, it was noted that the patient had signs of left facial droop. A CT scan was ordered. The CT demonstrated evidence of an acute hemorrhage in the right basal ganglia. Following the CT, the patient’s symptoms worsened and she became non-verbal. Naloxone was ordered, and the patient began thrashing in pain and pointing to her lower back. The physician who ordered the Naloxone arrived at the bedside and checked the patient’s blood pressure, which had become extremely elevated. The patient was sedated and then intubated. A subsequent CT revealed a large intraparenchymal hemorrhage and cerebral herniation. The following day, neurosurgery performed a craniotomy on the patient but she was declared brain dead shortly after the procedure.
Question(s) For Expert Witness
1. Do you routinely manage patients that present with cerebrovascular events in evolution?
2. What role would you conjecture Naloxone played in his deterioration if any?
Expert Witness Response E-036010
I am a full-time neurointensivist caring for patients at an academic medical center with catastrophic neurological illness and injury. I routinely manage such patients, as approximately one-third of our admissions to my 17-bed neuroscience ICU involve strokes in evolution, both acute ischemic strokes and intracerebral (ICH) hemorrhagic strokes. I have also given many teaching series and grand rounds on ICH to my colleagues in neurocritical care, residents, fellow neurologists, and medical students. In acute ICH the most critical parameter to control is blood pressure. Naloxone likely caused him an abrupt increase in pain (previously I presume on analgesics, which Naloxone reversed) which caused an acute rise in blood pressure, a known risk factor for expansion of an intracerebral hematoma. Current recommendations are to drop and maintain systolic blood pressure less than 140. The administration of Naloxone also likely delayed appropriate therapy.
About the author
Victoria Negron
Victoria Negron has extensive experience in journalism and thought leadership in the legal space, with a background crafting content, whitepapers, webinars, and current event articles pertaining to the role of expert witnesses in complex litigation matters. She is a skilled professional specializing in B2B product marketing and content marketing. Currently, she serves as an Enterprise Product Marketing Manager at Postman, and previously held the position of Technical Product Marketing Manager at Palantir Technologies, where she developed her skills in launch strategies, go-to-market strategy, and competitive analysis.
Her expertise in content marketing was further refined during her tenure at the Expert Institute, where she progressed from a Marketing Writer to Senior Content Marketing Manager, and eventually to Associate Director of Content & Product Marketing. In these roles, she honed her abilities in digital marketing, SEO, content strategy, and thought leadership.
Educationally, Victoria holds a Master of Business Administration from the University of Florida - Warrington College of Business and a Bachelor of Arts in Literature, Art, and Hispanic Studies from Hamilton College. Her diverse educational background and professional experience have equipped her with a robust skill set in product marketing, content development, and strategic marketing initiatives.