This case takes place in Indiana and involves a female patient with a past medical history of multiple chronic conditions. The patient had presented to the ER due to complaints of chest pain and shortness of breath. Once at the hospital, an abdominal x-ray was performed, which revealed a band of density in a small section of her lungs, however her lungs were otherwise clear. However, there was large amounts of stool intermixed with air throughout the colon, which was compatible with fecal impaction or constipation. Several additional tests were preformed at this point, one of which detected an elevated white blood cell count, however the patient was diagnosed with constipation and sent home.
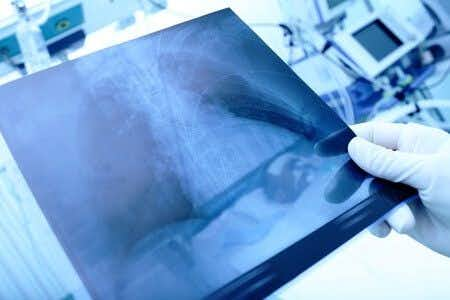
Some time after initially leaving the hospital, the patient presented to the ER again complaining of symptoms of dehydration. A chest x-ray showed massive right pneumonia. Antibiotics were started immediately, however she had a spiking fever and a diagnosis of severe sepsis and septic shock. The patient was admitted to the ICU, where she succumbed to her pneumonia and died.
Question(s) For Expert Witness
1. What is the normal work-up for a patient presenting with these signs and symptoms?
2. Should the patient have been discharged without her elevated WBC being addressed?
3. Had the patient's pneumonia been diagnosed sooner, could the outcome have been better?
Expert Witness Response E-007980
The only way to really know what the MDs were thinking is to read their notes from the ED. It's crucial to know if the spiral CT was done of the chest as well as part of an exclusion for pulmonary embolism. The CT would be much more sensitive than the CXR. The elevated WBC is nonspecific, and while it's tempting to imply that this was a forme fruste of pneumonia, I have personally been consulted many times for such a condition where the WBC is due to constipation and pain, and there are no dire consequences. I'm wondering why he was manually disimpacted, and why an enema was not given in the ED to facilitate improvement. It seems like a tall order to follow all those directions for constipation at home. It's also crucial to know what was happening with the patient in the 5 days between. Was he home vomiting, suggesting development of obstruction, and then developing aspiration pneumonia from this? This case would require teasing out the ED visit and follow up 5 days before the ED presentation.
About the author
Joseph O'Neill
Joe has extensive experience in online journalism and technical writing across a range of legal topics, including personal injury, meidcal malpractice, mass torts, consumer litigation, commercial litigation, and more. Joe spent close to six years working at Expert Institute, finishing up his role here as Director of Marketing. He has considerable knowledge across an array of legal topics pertaining to expert witnesses. Currently, Joe servces as Owner and Demand Generation Consultant at LightSail Consulting.