An infectious disease expert witness advises on a case involving a patient who died from sepsis. Decedent was treated in the defendant emergency room for a left swollen arm/hand/wrist with pain, generalized weakness, unsteadiness, some shortness of breath, and loss of appetite. He was diagnosed acute gout and discharged. Less than 2-days later, he was taken to another emergency room, where he was diagnosed with sepsis due to strep pneumonia, was intubated, and admitted to intensive care. His condition deteriorated and he died a week later.
The cause of death is listed as refractory asystolic cardiac arrest 5 minute duration, hemorrhagic myocardial infection one week duration, and pneumococcal infection/sepsis two week duration.
Decadent’s family filed a negligence action against the defendant emergency room in the Pennsylvania Court of Common Pleas.
Question(s) For Expert Witness
1. Would the patient have had a better outcome if he had been treated for sepsis during his initial emergency visit?
2. What else contributed to his death?
Expert Witness Response
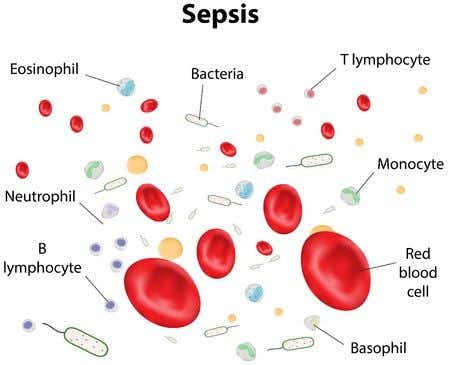
It is essential to emphasize the likelihood of severe morbidity and mortality at the time of the initial presentation of the patient when he presented with septic arthritis. He was found to be bacteremic with S. pneumoniae and so the question arises, what was the pathogenesis of the septic arthritis? It is unequivocal that septic arthritis involving S. pneumoniae is the result of bacteremia and may in turn have contributed to the perpetuation of the bacteremia. In other words, patient had been bacteremic prior to the initial presentation in the emergency department and the bacteremia is almost certainly the result of primary respiratory infection which was apparent but not diagnosed at the initial presentation. S. pneumoniae resides in the upper respiratory tract and generally causes pneumonia, which I believed the patient had at the time of the initial presentation.
He certainly had an abnormal chest CT scan when he was admitted later. Moreover, he never died from the septic arthritis, the critical factor which contributed to the patient's death was infective endocarditis with a devastating aortic valve infection. In all likelihood, this infection was also the result of the primary bacteremia secondary to the respiratory tract infection and it is more than likely that at the time of his first presentation with septic arthritis, that he already had cardiac valve involvement which progressed rapidly to cause his demise.
He almost certainly suffered from Austrian's syndrome which is a triad of S. pneumoniae causing pneumonia, infective endocarditis, and meningitis. He had all three and therefore fits this diagnosis perfectly. The implication of this understanding, is that even if he had received high dose antibiotic therapy at the time of his initial presentation to the ED, (where the diagnosis of septic arthritis was missed) that he already had bacterial dissemination to other sites and that one could not state with greater than 50% probability that he would have survived had he been given high dose IV antibiotics at the time. He had a high mortality syndrome at his initial presentation.
About the author
Kristin Casler
Kristin Casler is a seasoned legal writer and journalist with an extensive background in litigation news coverage. For 17 years, she served as the editor for LexisNexis Mealey’s litigation news monitor, a role that positioned her at the forefront of reporting on pivotal legal developments. Her expertise includes covering cases related to the Supreme Court's expert admissibility ruling in Daubert v. Merrell Dow Pharmaceuticals Inc., a critical area in both civil and criminal litigation concerning the challenges of 'junk science' testimony.
Kristin's work primarily involves reporting on a diverse range of legal subjects, with particular emphasis on cases in asbestos litigation, insurance, personal injury, antitrust, mortgage lending, and testimony issues in conviction cases. Her contributions as a journalist have been instrumental in providing in-depth, informed analysis on the evolving landscape of these complex legal areas. Her ability to dissect and communicate intricate legal proceedings and rulings makes her a valuable resource in the legal journalism field.