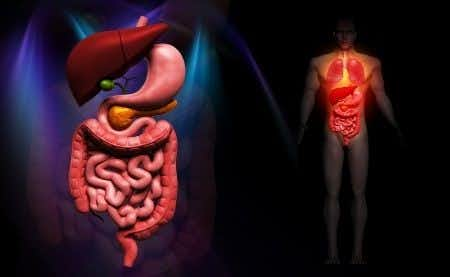
A hospitalist expert witness opines on the death of a patient from Oklahoma following a failure to detect a massive gastrointestinal bleed. This case involves a forty-seven-year-old male with a past medical history of drug addiction. The patient’s past medical history was also significant for hepatocellular carcinoma which was treated with chemoradiation ten-years prior. The patient presented to the hospital with complaints of right upper quadrant pain, vomiting, and dark blood in the stool for two weeks. The previous few day days prior to admission to the ER the patient experienced coffee-ground emesis and the inability to tolerate anything by mouth. The patient also reported being very constipated since he was started on a methadone regime. The patient had a previous right upper quadrant ultrasound a week ago prior to presentation. The ultrasound found no abnormalities. Several hours after the admission the patient experienced a severely hypotensive episode. The patient had a 20 gauge IV in place but the access was lost when the staff tried to infuse a bolus of fluids. The nursing staff tried to regain peripheral access over the next 20 minutes but without success. The patient was given a dose of Ativan to calm him and prevent respiratory alkalosis. The patient became unarousable shortly after and a code was called. Femoral IV access was finally obtained but the patient remained in a state of pulseless electrical activity for 16 minutes until time of death was called. The cause of death was cardiac arrest secondary to a large GI bleed.
Question(s) For Expert Witness
1. Should this massive GI bleed have been detected sooner?
2. Did the trouble in attaining IV access alter this patient's outcome?
Expert Witness Response E-005297
The patient’s history is concerning and would raise suspicion of a slow GI bleed, likely of upper origin. Depending on the clinical exam and suspicion, two large bore IVs should have been placed with STAT labs sent. His vitals, initial laboratory findings, and comparison to prior results will be essential in determining the likelihood of a GI bleed. Also, a NG lavage to rule out an upper GI bleed would have been indicated. Unless the laboratory and vitals were reassuring, the GI bleed could have likely been detected sooner. The symptoms warranted work up and management for massive GI bleed. Secondly, the standard of care for GI bleed is placing two large bore IVs and therefore in this case the IV access challenges were due to not meeting these standards. I am a hospitalist with significant experience taking care of gastrointestinal bleeds. I see 3 GI bleeds in a given week on inpatient service. IV access is always critical during a code situation. If suspicion was high in the beginning, multiple IV access sites should be placed. If there was a significant drop in pressure, IV access would be critical. Depending on the urgency, an IO could have been placed as well.
About the author
Dr. Faiza Jibril
Dr. Faiza Jibril has extensive clinical experience ranging from primary care in the United Kingdom, to pediatrics and child abuse prevention at Mount Sinai Hospital, to obstetrics in Cape Town, South Africa. Her post-graduate education centered on clinical research and medical ethics. Dr. Jibril is currently Head of Sales in the US and Canada for Chambers and Partners - a world leading legal ranking and insights intelligence company.