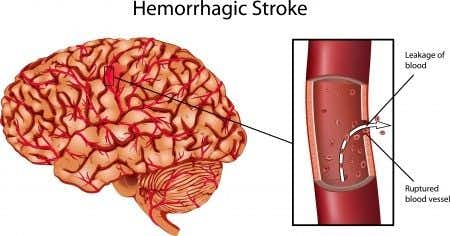
A hematology expert witness opines on post-operative anticoagulation in patients with multiple comorbidities. This case involves a fifty-four-year-old female patient with a past medical history of obesity and Atrial Fibrillation. The patient was being treated by her primary care physician and had been prescribed Coumadin for her arrhythmia. It was decided by her cardiologist that the patient required a cardiac ablation. The surgery was performed without complications; however in the post-operative recovery period the treating surgeons recognized that the patient required an emergent cholecystectomy. The procedure was initially intended to be performed laparascopically, however had to be converted to open technique due to complications intraoperatively. The surgery was completed and the patient was transferred to the PACU. Post-operatively, physicians had a difficult time controlling the patient’s PTT. The patient was given a large dose of Heparin on post-operative day six. She coded and died as a result of internal hemorrhaging.
Question(s) For Expert Witness
Are you familiar with post op Heparin guidelines for a patient in this condition?
Expert Witness Response E-008453
This is a scenario I encounter frequently in my practice, a patient at simultaneous risk for clotting (stroke from atrial fibrillation, obesity) and for bleeding (recovering from an open cholecystectomy). My clinical practice focuses on the diagnosis and management of bleeding and clotting disorders, particularly in unique populations such as pregnant women and critically ill hospitalized patients. Deciding whether to give heparin in a scenario like this is complicated because either withholding or administering anticoagulation carries risks, and these risks need to be discussed with the patient and family, all treating physicians, and thoroughly documented in the medical records. Doctors frequently either fail to have this conversation, or do not adequately document the risks and benefits of anticoagulation (and the fact that they were discussed with the family and other treating physicians), in the medical record.
The annual risk of stroke for patients with atrial fibrillation who do not receive anticoagulation is about 5%, meaning that the risk of stroke if someone does not receive treatment for a week is less than 1%. Doctors often do not appreciate this and may insist on administering heparin to patients who are at high risk for bleeding. This is an inappropriate approach. When evaluating this case, it would be important to assess whether the doctors had the conversations outlined above with the patient and family, and if heparin was administered correctly. It will also be important to determine if the presence of bleeding was adequately assessed.
About the author
Dr. Faiza Jibril
Dr. Faiza Jibril has extensive clinical experience ranging from primary care in the United Kingdom, to pediatrics and child abuse prevention at Mount Sinai Hospital, to obstetrics in Cape Town, South Africa. Her post-graduate education centered on clinical research and medical ethics. Dr. Jibril is currently Head of Sales in the US and Canada for Chambers and Partners - a world leading legal ranking and insights intelligence company.