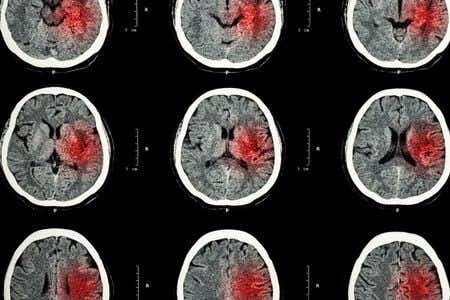
This case takes place in Washington and involves a male patient who presented to the ER with complaints of neck pain and nausea. He underwent multiple scans and diagnostic tests, all of which appeared to be negative for major injuries or potential causes for his symptoms. As a result of these findings, the patient was prescribed painkillers and instructed to return if his symptoms became worse. Several days later, the patient presented to the ER again with complaints of increased neck pain, as well as continuing nausea. His treating physicians discharged him again after prescribing a higher dose of painkillers. A few days later, the patient was rushed to a different hospital after being found unconscious on his kitchen floor. A new round of scans were performed which revealed the presence of a significant hemorrhage in his brain, at which point the patient was admitted for emergency surgery. It is alleged that the initial scans were not reviewed correctly, and that the patient should have received appropriate treatment much sooner.
Question(s) For Expert Witness
1. Do you see patients with this type of presentation? If so, how often?
2. What is the standard work up for patients with these signs and symptoms?
3. What is the differential diagnosis for this type of presentation?
4. What follow up should be ordered to monitor a patient with these symptoms?
Expert Witness Response E-006248
This is an extremely common patient presentation that I see on a very frequent basis, at least once per shift. The standard workup for this presentation varies widely. In some cases, a thorough history and physical will provide enough diagnostic information; in others, laboratory and radiologic studies are indicated. In this case both CT and MRI were performed, suggesting that the ordering clinician had a high index of suspicion for significant pathology. Neck and back pain, diaphoresis, and nausea are relatively non-specific complaints that have an extremely large differential diagnosis. Further history and physical exam information would help begin the narrowing process but, to begin with, a differential might include: meningitis, vertebral or carotid artery dissection, intracranial bleed, aortic dissection/aneurysm, myocardial infarction, esophageal/pharyngeal rupture, pulmonary embolus, soft tissue neck infection including cellulitis, abscess and necrotizing infection, fracture or other traumatic injury, spinal stenosis, syrinx, neuropathy, spinal infarct, and pneumonia. Follow up to monitor such a patient would really depend on their condition at discharge. If pain had not been controlled adequately in the emergency department, admission to an inpatient bed for both pain control and 24 hour observation may have been warranted. If pain could be controlled adequately, follow up within 24 hours for recheck would usually be the standard of care given the clear extensive nature of the pain and the clear clinical concern of the treating physicians who ordered extensive diagnostic testing.
About the author
Joseph O'Neill
Joe has extensive experience in online journalism and technical writing across a range of legal topics, including personal injury, meidcal malpractice, mass torts, consumer litigation, commercial litigation, and more. Joe spent close to six years working at Expert Institute, finishing up his role here as Director of Marketing. He has considerable knowledge across an array of legal topics pertaining to expert witnesses. Currently, Joe servces as Owner and Demand Generation Consultant at LightSail Consulting.