A bariatric surgery expert witness opines on a case where a patient died as a result of small bowel obstruction following initial discharge after conservative management. This case involves a thirty-eight-year-old female patient who presented to the ER complaining of severe abdominal pain for the past two days, nausea and vomiting. The patient was admitted to the hospital in Oklahoma for five days with a diagnosis of partial bowel obstruction and was discharged following conservative treatment. The patient had a past medical history significant for multiple abdominal surgeries for hernia repair, morbid obesity and a current ventral hernia. At the time of her admission she was undergoing evaluation at another facility for bariatric surgery as an intervention for her obesity. She returned to the hospital one day following discharge with feculent vomitus. The patient was admitted with an incarcerated ventral hernia, small bowel obstruction, and persistent abdominal pain. Her symptoms did not improve following conservative treatment and the decision was taken to the operating room for an exploratory laparotomy. This procedure resulted in the repair of incarcerated ventral hernia with Composix graft mesh. Postoperatively, it was decided to leave the patient intubated. She became hypotensive postoperatively and spiked a temperature of 102 degrees F. The patient remained intubated and required vasopressors to maintain her blood pressure. She became progressively more hypoxic, developed bilateral pleural effusions, and was acidotic. A week after surgery, the patient’s endotracheal tube became dislodged after the balloon burst. The patient was unable to be resuscitated and succumbed to her medical conditions.
Question(s) For Expert Witness
1. Was it appropriate to discharge the patient after her partial bowel obstruction hospitalization?
2. Was prolonged intubation indicated in this case?
Expert Witness Response E-001161
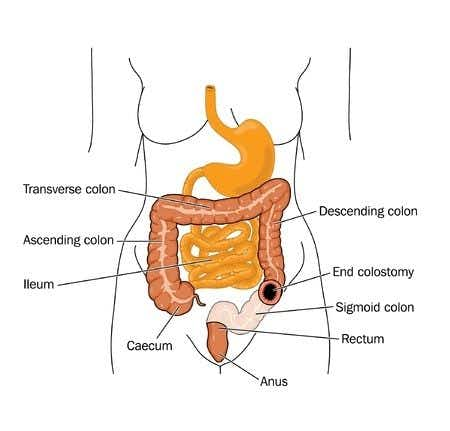
Acute small bowel obstruction is an interruption in the forward motion of intestinal contents through the small bowel. The patient in this case is the classic clinical presentation of the condition which includes nausea and vomiting, colicky abdominal pain, and inability to pass gas or stool. Conservative management of uncomplicated intestinal obstructions includes fluid resuscitation with correction of metabolic derangements, intestinal decompression, and bowel rest i.e. nil by mouth regimen. Patients discharged after small bowel obstruction who are treated conservatively must follow specific guidelines that prove that the obstruction has adequately resolved. A thorough review of the patient’s medical records would reveal if that was or was not the case here. Typically, patients are evaluated for a tracheostomy if prolonged intubation is necessary to prevent the complications of prolonged complications. Depending on her clinical factors, the patient may have needed a tracheostomy, which would have prevented the complication of ETT balloon bursting.
About the author
Dr. Faiza Jibril
Dr. Faiza Jibril has extensive clinical experience ranging from primary care in the United Kingdom, to pediatrics and child abuse prevention at Mount Sinai Hospital, to obstetrics in Cape Town, South Africa. Her post-graduate education centered on clinical research and medical ethics. Dr. Jibril is currently Head of Sales in the US and Canada for Chambers and Partners - a world leading legal ranking and insights intelligence company.